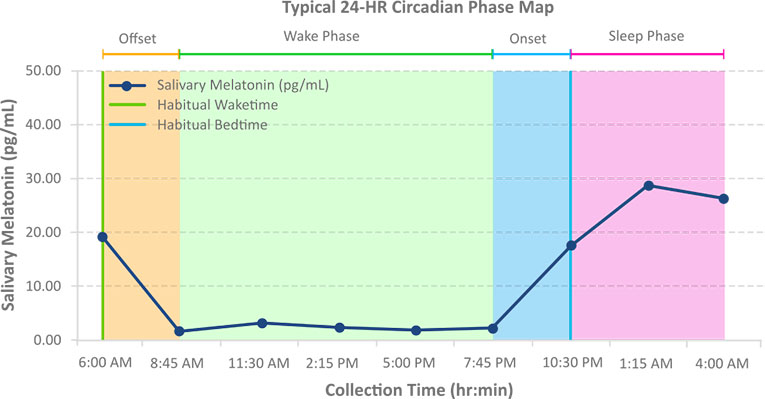
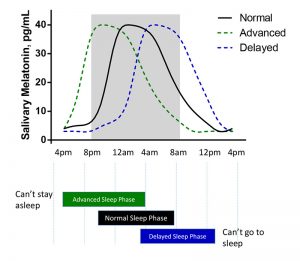
Normal Sleep Onset
Typically, the melatonin onset should occur around two hours before bedtime, when melatonin levels have increased significantly enough to begin the sleep process. Some sleep disturbances are non-circadian sleep disorders and may not be directly tied to a sleep phase shift. A robust peak melatonin level and low baseline or waking level are both important aspects of a normal sleep onset. Normal Sleep Phase results need to be considered in the context of the patient’s overall presentation and available diagnostic data.
Phase Advanced
An advanced sleep phase, indicated by a DLMO that is earlier than ~3 hrs before habitual bedtime and an offset that is ~3 earlier than wake time, is often seen in individuals who have difficulty staying awake until their desired bedtime in the evenings and often have problems staying asleep in the early morning hours. Often, therapy involving strategically timed exposure to blue light can inhibit melatonin production and delay the onset until the patient’s desired bedtime.
Phase Delayed
A delayed sleep phase, indicated by a DLMO that is later than ~1 hrs before habitual bedtime and an offset this is later than ~3 hours post-waking, is often seen in individuals who have problems falling asleep at their desired bedtime and difficulty waking up in the morning. Here, strategically timed treatment with proper melatonin supplementation can pinpoint the necessary increase in melatonin levels to help patients fall asleep at their desired bedtime.
No Onset / Undetermined
In profiles where the threshold is never crossed, such as flat-line results or atypically elevated levels, the interpretation of the DLMO cannot be calculated. This may indicate poor sleep hygiene, poor circadian entertainment, pharmacological disruption, psychiatric conditions, or low levels of daytime light exposure. Atypically elevated thresholds can occur if one or more of the first 3 baseline values are abnormally elevated. Retesting is recommended for accurate results, ensuring careful adherence to test instructions.
Baseline Average
A high or elevated baseline indicates that melatonin levels were rising prior to the beginning of sampling. In this case, patients may have entered into a dim light area early or may be experiencing dysregulation from abnormal daytime levels of melatonin, often caused by supplementing higher doses than required. An interesting observation is the slow clearance of supplemental melatonin relative to endogenously produced melatonin. Supplements can cause high melatonin levels (above 50 pg/ml) for up to 10 days depending on the dose taken. These supplements can affect a person’s chronotype which has also been described as a melatonin hangover.
Peak Level
The peak level reported during the sampling regimen can be an important indication of sufficient melatonin production. A low peak level can indicate a suppressed melatonin onset and can result from inadequate daytime light exposure, cataracts, or poor sleep hygiene related to blue light exposure from screens or other sources. Children and adolescents should have very robust melatonin peak levels, in some cases above 50 pg/ml. Melatonin peak levels may also decrease with age.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)